Tom Burns, who I have mentioned in a
previous post, has written a bland apology for psychiatry,
Our necessary shadow: The nature and meaning of psychiatry. As he says, he is "convinced psychiatry is a major force for good or I would not have spent my whole adult life in it". Having also spent most of my adult life as a psychiatrist, I suppose I'm inclined to be an apologist as well, but I would only say that psychiatry can do good not that it does. Burns recognises what he calls psychiatry's "mistakes" but sees these as failings that need to be put in perspective, rather than, as I do, something more fundamental about the nature of psychiatry.
Burns describes a new group of anti-psychiatrists, which he says "are, as it were,
evidenced-based anti-psychiatrists" [his italics]. In this group he selects from what he calls an "almost endless" list of books: Richard Bentall's
Doctoring the mind (see my
previous post) and
Madness explained; Jo Moncrieff's
The myth of the chemical cure (see my
post about Jo's new book); and Peter Breggin's
Toxic psychiatry and
Brain disabling treatments in psychiatry. (See my
book recommendations on my critical psychiatry website.)
Burns suggests these new anti-psychiatrists (see
previous post about use of the term 'anti-psychiatrist'), although they may share "a deep suspicion of the fundamental legitimacy of psychiatry and psychiatric diagnoses" are more concerned about "the
damage done by psychiatry and psychiatrists" [his italics]. From his point of view, "their arguments are generally that psychiatry is too full of itself, or is corrupted by pharmaceutical companies, or that it makes endless mistakes". One of his reasons for writing his book is to "try and explain why psychiatry survives despite this tsunami of criticism". He goes on:
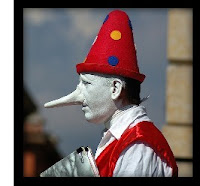
If psychiatrists are false prophets it is because they fail to deliver what they promise; it is not their mistaken metaphysics. It is their incompetence rather than their omnipotence that is the issue.
If I understand him right, he doesn't want to engage with conceptual issues about the nature of mental illness. This is not dissimilar from the position of Anthony Clare in
Psychiatry in dissent (see
previous post) and fits with Burns ambition to see his book as this generation's "attempt to explain psychiatry fully to the interested outsider", as Clare's book was for a previous generation. I think Burns is setting the barrier of competence too high for psychiatrists! He clearly does have an ideological position eg. he accepts the rather trite position that schizophrenia has a heritability of 80%. Despite what he thinks, as I keep saying, it is important to move on from the biomedical paradigm (see
previous post). Burns atheoretical approach does not salvage psychiatry.